The Penridge Suite, London, N11 1NL, UK : Friday, 14th Oct 2011 09:00 - 17:00
The gut epithelium is continually exposed to diverse dietary and environmental antigens in the presence of commensal bacteria. Yet, in the face of this multitude of ‘foreign’ antigens, the gut is able to maintain a state of non-responsiveness while able to react to true pathogens that invade the gut mucosa. This capacity is thought to be acquired through complex interactions between the gut microbiota, intestinal epithelium and underlying mucosal immune system. While dendritic cells (DCs) are likely to play a crucial role in this homeostasis through their linkage of innate with adaptive immunity, intestinal epithelial cells are currently attracting considerable attention for their expression of a range of factors that could influence the behaviour of DCs, thereby shaping the ensuing response. The scope of this meeting is to assimilate current knowledge of the role of epithelial cells in the dialogue that occurs at mucosal surfaces.
This event has CPD accreditation and will have a discussion panel session.
Meeting chairs: Dr. Kamal Ivory, Institute of Food Research,Norwich, UK and Professor Claudio Nicoletti, Norwich Research Park, United Kingdom
9:00 – 9:45 Registration
9:45 – 10:00 Introduction by the Chairs: Dr. Kamal Ivory, Institute of Food Research, Norwich, UK and Professor Claudio Nicoletti, Norwich Research Park, United Kingdom
10:00 – 10:30 The Big Society: local immune regulation by human mucosal antigen presenting cells in the human intestinal mucosa
Dr Andrew Stagg, Barts and The London School of Medicine and Dentistry, Centre for Immunology and Infectious Disease, Blizard Institute of Cell and Molecular Science, London
The intestine is a highly active immune organ. To protect against pathogen colonisation, the local immune system must sample and respond to luminal contents. In health, reactivity to the commensal microbiota is restrained by regulatory mechanisms that prevent the development tissue damage. However, in inflammatory bowel disease (IBD) dysregulation of these pathways leads to chronic inflammation. This talk will focus on the role of diverse antigen presenting cells, acting in draining lymphoid tissue to shape the development of T cell responses and locally in the mucosa to regulate effector function, in the regulation of intestinal immune responses.
10:30 – 11:00 Oral Mucosa: Gatekeeper or housekeeper?
Dr. Lesley Ann Bergmeier, Centre for Clinical and Oral Diagnostic Sciences, Institute of Dentistry,Queen Mary’s Schools of Medicine and Dentistry, UK
The oral mucosa can be regarded as a quiescent environment with little inflammatory activity to drive either innate or adaptive immune responses. However, this belies its capacity to respond to antigenic stimuli in either a response to the inflammation associated with common oral diseases (caries and periodontal diseases) or its ability to tolerate the vast amount of material to pass through the mouth as food or indeed in response to the extreme environmental changes associated with heat , cold, alcohol and tobacco intake. The oral mucosa is very far from being inactive.
11:00– 11:30 Mid-morning break and Poster Viewing
11:30 – 12:00 Crosstalk between intestinal epithelial cells and intraepithelial lymphocytes
Dr Lucie Abeler-Dorner, Kings College, London
Throughout the small intestine, epithelial cells (IEC) are in close contact with intraepithelial lymphocytes (IEL). IEL constitute one of the largest T cell compartments, but are commonly excluded from models of gut immune function. Making use of a novel system to culture IEL in vitro, we identify a hitherto unrecognized cytokine collaboration by which IFNγ, TNF and IL-1α produced by activated IEL provoke IEC to increase IL-6 production. Elevated IL-6 levels in the gut are associated with increased epithelial cell turnover, inflammation and carcinogenesis. This newly identified IEL:IEC cross-talk offers a novel source of factors regulating mucosal homeostasis, infection, and pathology.
12:00 – 12:30 Intra-hepatic immune regulation
Professor David Adams, University of Birmingham, Birmingham, UK
The liver is a major site of immune regulation capable of supporting vigorous immune responses against some pathogens but also able to promote tolerance to food antigens. Local immune regulation is controlled by distinct populations of antigen presenting cells which inlcude hepatic endothelial cells and epithelial cells as well as dendritic cells and regulatory T cells. Understanding the complex intrahepatic immune environment will elucidate the pathogenesis of persistent infection in hepatitis B and C infection and the breakdown in tolerance that leads to autoimmune liver disease.
12:30 – 13:00 Intestinal dendritic cells in mucosal clearance: a new defence mechanism?
Angela Man, Institute of Food Research, Norwich, UK
13:00 - 14:00 Lunch, and Poster Viewing
14:00 - 15:00 Question and Answer Session and Speakers photo
Delegates will be asked to submit questions to a panel of experts. Questions can be submitted before the event or on the day
15:00 - 15:30 Afternoon Tea/Coffee, and Last Poster Viewing
15:30 – 16:00 Dissecting the Crosstalk Between the Intestinal Epithelium and Dendritic Cells: Dendritic Cell Mobilisation in Infection
Dr Sheena Cruickshank, Manchester Immunology Group, Manchester, UK
The ability of the colon to generate an immune response to pathogens is a fundamental and critical defence mechanism. We use enteric pathogens such as Trichuris muris to dissect the crosstalk between external signal (pathogen), epithelial cell and immune cell. This talk will discuss our work on epithelial mediated recruitment of dendritic cells in the gut and the implications of dendritic cell recruitment in resistance to infection.
16:00 – 16:30 Dendritic cells and the respiratory epithelium
Dr Andrew Thorley, National Heart and Lung Institute, Imperial College London, UK
The respiratory epithelium is often overlooked as a key player in the host pulmonary immune response; many believe it to be merely a barrier with little or no ability to respond to pathogenic or pro-inflammatory material. This talk aims to highlight the important role epithelial cells play in initiating and orhcestrating immune responses to infection and inhaled toxicants via release of cytokines and chemokines which drive dendritic cell recruitment and maturation.
16:30 – 17:00 Chairman’s summing up
Media Partners
About the chairs
Dr Kamal Ivory is a project scientist in the Mucosal Immunology group at the Institute of Food Research in Norwich. She began her research career looking at ways to prevent kidney allograft rejection at Guy’s Hospital in London. From there Kamal moved to the Royal Free Hospital (RFH) where she obtained her PhD. She continued to work there on ways of exploiting the potential of monoclonal antibodies for diagnosis and therapy, while also participating in ageing and immunodeficiency research. On moving to the Institute of Food Research in Norwich Kamal initially worked on healthy ageing, but is currently studying immune regulation in food allergy
About the Speakers
Lesley Ann Bergmeier joined the Centre for Clinical and Diagnostic Oral Sciences at Queen Mary University of London as Senior Lecturer in Applied Mucosal Immunology in November 2006. She has spent her career in the field of mucosal immunology focussing on vaccine design and the interface between innate and adaptive immunity at mucosal surfaces. Prior appointments were as researcher and then lecturer at Kings College London. Currently her interests include the chaperokine functions of heat shock proteins and their role in immune homeostasis in the oral cavity, with particular reference to disregulation at the oral mucosa.
David Adams is director of the Centre for Liver Research and the NIHR Biomedical Research Unit for Liver disease at the University of Birmingham. His clinical interests are transplant hepatology and autoimmune liver disease. Laboratory research focuses on mechanisms of immune-mediated liver disease. After initial training in hepatology in Birmingham he continued his immunology training with Dr Stephen Shaw at the Experimental Immunology Branch of the National Cancer Institute, Bethesda, USA; he was appointed to the Chair of hepatology in Birmingham in 1997. He was made a Fellow of the Academy of Medical Sciences in 2000. His group has defined molecular mechanisms that control the entry of leukocytes from the blood and they are now translating this information to develop cell therapy for liver disease in which dendritic cells and regulatory T cells are used to manipulate immune responses in patients in vivo.
Dr Andrew Thorley is an Academic Fellow in the Lung Cell Biology Group at the National Heart and Lung Institute. Dr Thorley graduated from the University of Bath with a Masters in Pharmacology and subsequently joined the Lung Cell Biology group at the National Heart and Lung Institute to undertake a PhD investigating the role of alveolar macrophages, dendritic cells and respiratory epithelial cells in lung inflammation, with a particular focus on Toll-like receptor activation and bacterial infection. Dr Thorley has continued his research at Imperial College by developing his work on Toll-like receptors, investigating the effects of cigarette smoke and nanoparticles on the inflammatory response of the peripheral lung.
Sheena Cruickshank joined the The University of Manchester in 2007 as a lecturer. She started her research in enteric parasitic infections in Glasgow before moving to Cancer Research UK where she did her PhD on epithelial/lymphocyte interactions in autoimmune liver disease. Her postdoctoral research experience was with Cancer Research UK and the University of Leeds and it was here that her interest in dendritic cell function first developed. Current work in her group is addressing the interaction of epithelial cells with dendritic cells and other innate cells in the context of infection, inflammation and delayed wound healing.
Lucie Abeler-Dörner joined King’s College London as a postdoctoral research fellow in 2008 after having received her PhD from the University of Heidelberg. Her research interests include mucosal immunology, immune surveillance and tissue-specific immune regulation. Having worked on the tolerization of dendritic cells by apoptotic cells before, her current research focuses on the crosstalk between intestinal epithelial cells and intraepithelial lymphocytes during the steady state, innate stress responses and food allergy.
Dr Andy Stagg is Senior Lecturer in Immunology in the Blizard Institute, part of Barts & The London School of Medicine at Queen Mary University of London (QMUL). He obtained a PhD from the National Institute for Medical Research and worked as a postdoc in the Clinical research Centre and University of Texas Southwestern Medical Center before joining QMUL from Imperial College London in 2007. He has a longstanding interest in immune regulation by dendritic cells and other antigen presenting cells at mucosal sites and his current research focusses on the human intestine in health and in inflammatory bowel disease (IBD).
Keywords: Intraepithelial lymphocytes, IEL culture, IEL:IEC crosstalk,lung, infection, epithelium, smoking, chemokines, IL-6, epithelial cell, dendritic cell, colon, infection
Dont forget to sign up to Euroscicons’ e-newsletter at www.euroscicon.com/signup.htm to keep up to date with European Life Science news and events and to be notified of the follow up to this event
Registration Web Site: www.regonline.co.uk/mucosal2011
POSTERS
Intestinal dendritic cells in mucosal clearance: a new defence mechanism?
Angela Man, IFR, Norwich.
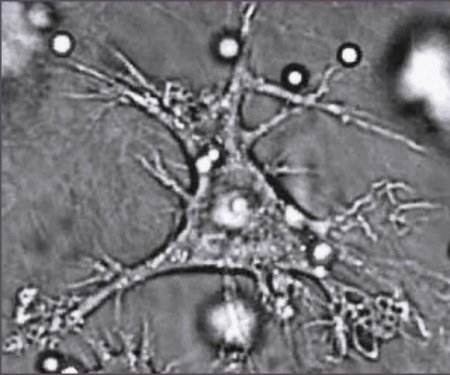
The intestinal epithelium forms a barrier with an overlying mucous layer harbouring a reservoir of secretory IgA (sIgA); in a process of immune exclusion, bacteria, viruses and macromolecules are prevented from entering the body. The epithelium also participates in monitoring luminal contents (LC) by providing access of the immune system to LC, in a process of antigen sampling. Recently, it was proposed that dendritic cells (DC) can form cellular extensions between epithelial cells and into the intestinal lumen, internalise bacteria and shuttle them across the epithelium. This mechanism complements the well-studied M-cell mediated transport of particulate antigen and bacteria that occurs in the follicle associated epithelium (FAE) of Peyer’s patches. We have previously shown that DC-mediated sampling is not the sole event occurring at the host-microbe interface in the gut in the presence of pathogenic bacterial stimulus (Salmonella). Indeed, following challenge with non-invasive Salmonella, we found a proportion of DCs rapidly migrate to, and across the lamina propria (LP) into the gut lumen, before or following internalization of Salmonella. Migration of this specific DC population (CD11c+ CX3CR1+ MHCII+ CD11b− CD8α−) was a flagellin- and MyD88-dependent process only observed in the small intestine. Most importantly, these intraluminal DCs captured bacteria, but did not cross the epithelium to return into the tissue, suggesting that these DC did not play a role in conventional antigen presentation. These data prompted us to extend our investigation into the role of DCs that transmigrated into the lumen. We hypothesised that Salmonella-capturing DCs represent a cell-based mechanism of immune exclusion, complementing the one formed by mucous and sIgA. By using mouse strains that differed in ability to perform DC-mediated sampling, we established that antigen translocation to the LP and mesenteric lymph node did not vary between DC-sampling competent (C57BL/6) and DC-sampling deficient (Balb/c and CX3CR1-/-) mice; thus suggesting that DC-sampling plays no significant role in antigen sampling in the gut . Parallel experiments also established that mice, that do not display intraluminal DC-migration in response to Salmonella, showed lower level of resistance to Salmonella infection. Although this is work in progress, we interpret these data as showing that DC-migration plays a role in mucosal clearance and also, our data questions the biological relevance of DC-mediated sampling.
Connect with us on
Nature network - http://network.nature.com/groups/euroscicon/
- http://www.linkedin.com/groups?gid=1939569
- http://www.facebook.com/group.php?gid=70847076549
- http://twitter.com/Euroscicon/
Post expires at 7:07am on Friday October 14th, 2011