The Penridge Suite, 470 Bowes Road, London N11 1NL
Friday, 11 March 2011 09:00 - 17:00
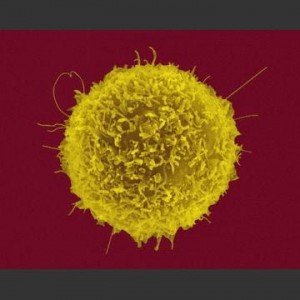
Autoimmune diseases affect up to 5% of Westernised populations and there is a pressing need to understand the underlying immunological mechanisms in order to design effective, targeted approaches to treatment. A key to such progress will be to determine why self-tolerance is lost in these conditions, and how it can be restored therapeutically. The recognition that various forms of regulatory cell have important roles in suppressing unwanted or damaging immune responses, including those that drive autoimmune disease, now provides an opportunity to achieve these goals. The meeting will discuss the identities and functions of regulatory cells, including the widely studied CD25+ T cell subset, their roles in disease, and how they could potentially be manipulated as therapeutic targets.
Meeting chairs: Dr Claudia Mauri, UCL, London, Professor Robert Barker, University of Aberdeen
This event has CPD accreditation and will have a discussion panel session.
On registration you will be able to submit your questions to the panel that will be asked by the chair on the day of the event
9:00 – 9:45 Registration
9:45 – 10:00 Introduction by the Chair: Dr Claudia Mauri, UCL, London
10:00 – 10:30 Regulatory cells in autoimmunity
Dr Claudia Mauri, University College London, UK
Over the last decade regulatory T cells have been considered the predominant, if not the only, population of lymphocytes capable of ameliorating autoimmune diseases, and acting as powerful suppressors of the activation of the autoreactive lymphocyte response. We and others have demonstrated that, in addition to Tregs, a discrete subset of B cell, namely regulatory B cells, possess equal suppressive capacity and inhibit inflammatory responses via the provision of IL-10. I will discuss our findings showing that the IL-10 produced by Bregs is important in the maintenance of the number of FoxP3+Tregs and IL-10+FoxP3-Tr1 cells whilst suppressing Th1/Th17 responses. I will also discuss how the mechanisms discovered in experimental models of autoimmunity operate in healthy individuals whilst they are defective in patients with autoimmunity.
10:30 – 11:00 Regulatory T-cells as biomarker in rheumatoid arthritis patients
Dr Frederique Ponchel, Leeds Institute of Molecular Medicine, UK
It is essential to predict the evolution towards rheumatoid arthritis (RA) from early symptoms in order to treat patients with the most appropriate drug regime to induce remission. The presence of autoantibodies to citrullinated protein (ACAP) is an essential biomarker however only present in 50% of early RA patients (ACPA+). We have previously reported that CD4+CD25high Treg are reduced in frequency in early RA with recovery in remission (Lawson 2006). Furthermore, CD62L+ Treg are predictive of successful cessation of TNF-inhibitor therapy (Saleem 2010). The aim of the current study is to determine whether Treg phenotyping can predict evolution towards inflammatory arthritis (IA) in ACAP+ individual with recent onset of musculoskeletal pain (arthralgia), discriminate early between IA patients with Undifferentiated Arthritis (UA) or RA evolution and predict remission and/or lack of response to early therapy. We used 6 colour flowcytometry to monitor Treg frequency (CD3+CD4+CD25highFOXP3+CD127low) and phenoptype (CD62L+/-) in different cohorts. The development of clinical synovitis within 12 months follow-up was observed in 36% of ACPA+ individuals with arthralgia (n=42); the other patients remaining arthralgia only. Baseline Treg frequencies were not significantly reduced in ACPA+ arthralgia patients compared to controls (n=55) neither in any particular outcome. In contrast, CD62L+ Treg were less frequent in individual evolving to UA (P=0.05) compared to RA. The arthralgia only patients had variable CD62L+ frequency different from RA (P=0.05) but not UA. 70 patients with <12 months IA were enrolled. Using newly developed 2010-RA criteria for diagnostic, 49 of the 70 patients evolved to RA, 11 remaining UA. Treg were reduced in the UA group compared to controls (P=0.028) but not significantly in RA. CD62L+ Treg were reduced in both UA (P=0.05) and RA (P=0.001) compared to health. 28 IA patients with <12 months symptom duration were recruited and treated with MTX only with the aim of inducing remission (treat to target concept). Treg did not predict the induction of remission at 6 months but a trend for low Treg was observed in patients lack of response (P=0.06). No significant difference were observed for CD62L+Terg. 32 IA patients with <12 months symptom duration were recruited and treated with MTX+TNF-inhibitor. Treg did not predict remission but lower frequency of CD62L+Treg did (P=0.033) at 6 months. Altogether these data even if preliminary suggest that regulation is perturbed early in the development of IA. Loss of Treg ability to circulate to lymph node (CD62L- Treg) may be an important step in evolution towards RA.
11:00 – 11:10 Speakers’ photo
11:10 – 11:30 Mid-morning break
11:30 – 12:00 Using biologic therapy to understand and reverse abnormal immune regulation in inflammation
Professor Michael Ehrenstein, University College London, UK
Biologic therapies not only offer the prospect of improved patient outcomes in a variety of autoimmune diseases, but also the opportunity to explore the specific target’s role in the underlying mechanisms of disease. Over recent years we have studied the role of regulatory T cells (Treg) in patients with rheumatoid arthritis before and after anti-TNF therapy. We have shown that Treg from patients with rheumatoid arthritis have defective suppressor function. This Treg defect is linked with abnormalities in the expression and function of CTLA-4. Anti-TNF antibody therapy did not reverse CTLA-4 dysfunction but instead induced the differentiation of a distinct and potent Treg population. These induced Treg were able to inhibit IL-17 production, in contrast to Treg from healthy individuals, patients with active RA or RA patients treated with etanercept, a modified TNF receptor. These results may provide mechanistic insight into the therapeutic benefit of switching between different anti-TNF agents and the differing incidence of tuberculosis between adalimumab and etanercept.
12:00 – 12:30 Cross-talk between CD4+ T cell subsets and monocytes
Dr. Leonie Taams, King’s College London, UK
Overwhelming evidence exists that naturally occurring regulatory T cells (Tregs) play a pivotal role in the regulation of immune responses, both in mouse models and in humans. Naturally occurring Tregs are present in the blood and (non) lymphoid tissue of healthy humans, where they comprise approximately 2% of all CD4+ T cells. The suppressive effects of Tregs on the adaptive immune response are well established; however their effects on cells from the innate immune system are less well defined. Our lab is particularly interested in the functional consequences of the interactions between monocytes, CD4+CD25+ Tregs and CD4+CD25- responder T cells, in the steady-state as well as during disease. We recently highlighted a novel function of Tregs, by showing that these cells exert direct suppressive effects on monocytes resulting in impaired T cell-stimulatory capacity, a reduced ability to respond to Toll-like receptor agonists and an alternatively activated phenotype. We believe that this outcome is important for the maintenance of immune homeostasis, however when dysregulated, it may result in chronic inflammation or cancer. Our current work is aimed at identifying the molecular pathways underlying the Treg-induced anti-inflammatory function of monocytes/macrophages, using gene expression profiling and biochemical analysis of signal transduction pathways.
12:30–13:30 Lunch
13:30 – 14:30 Question and Answer Session: Chair: Professor Robert Barker, University of Aberdeen
Delegates will be asked to submit questions to a panel of experts. Questions can be submitted before the event or on the day
14:30 – 15:00 How do Treg use CTLA-4 to control autoimmune tissue destruction?
Dr Lucy Walker, University of Birmingham Medical School, UK
We have known for 15 years that mice lacking CTLA-4 have over-active immune systems resulting in lethal pathology. This reveals CTLA-4 to be an essential mediator of peripheral T cell tolerance. Nevertheless, a clear understanding of which cells CTLA-4 works on, and indeed how it works, is lacking. We have addressed these questions using a combination of in vivo and in vitro approaches. Using an adoptive transfer model of diabetes, we show that CTLA-4 expression on Treg is essential for effective disease regulation. Experiments addressing the molecular basis of CTLA-4 function will be presented.
15:00 – 15:30 Talk title to be confirmed
Dr Marc Veldhoen, Cambridge, UK
15:30 – 16:00 Afternoon Tea/Coffee
16:00 – 16:30 iNKT cells in autoimmunity: lessons learnt from SLE patients before and after B cell depletion therapy
Dr Liz Jury, University College London, UK
iNKT cells exert a critical function in a broad range of immune responses including protection from specific pathogens, tumors and maintenance of tolerance in autoimmunity. Given the pleiotropic function of iNKT cells, and their potential for therapeutic applications, great interest exists in elucidating the mechanisms controlling iNKT cell development and activation. Changes in iNKT cell frequency have been reported in patients with autoimmune disease. However whether iNKT cells are also functionally defective remains to be ascertained. Our work with SLE patients before and after B cell depletion therapy has lead us to propose that “healthy” B cells are pivotal in the physiological maintenance of iNKT cell number and function.
16:30 - 17:00 Role of Treg cells and T cell homeostasis in lupus: evidences for their therapeutic potency
Professor Gabi Riemekasten, Schwerpunkt Rheumatologie und Klinische Immunologie, Germany
Effector T cells play an important role in the pathogenesis of lupus and, as recently shown in murine lupus, they contribute to tissue damage and glomerulonephritis. In healthy individuals as well as in young lupus prone mice without any signs of the disease, effector T cells are tightly controlled by naturally occurring regulatory T cells (Treg) that can be shown by different approaches: 1. After depletion of Treg cells by anti-CD25 therapy, murine lupus is strongly accelerated. 2. After passive transfer of Treg (CD4+CD25+ T cells consisting of 95% FoxP3+ T cells) murine lupus improved reflected by reduced proteinuria and increased survival compared to control mice. The control of effector T cells by Treg cells can be also used for studying the phenotype of effector T cell and their function at an autoantigen-specific level. Depletion of Treg cells by MACS unmask effector. T cell reactivity to an autoantigen and can allow the better characterization of effector T cells under certain disease conditions. However; as shown in the murine NZB/W lupus model, there is a progressive loss of Treg/Tcon homeostasis during lupus development in different compartments with a progressive Treg deficiency. In lupus mice with proteinuria, the phenotype of effector T cells is very similar to the T cell phenotype obtained in IL-2 deficient mice. According to the characteristics of Treg, they are more sensitive to IL-2 deficiency. Supporting this, addition of IL-2 resulted in a dominant proliferation of Treg cells leading to improvement of murine lupus. Our data support the possible role of Treg and of IL-2 in the therapy of lupus.
17:00 Chairman’s summing up: Professor Robert Barker, University of Aberdeen
Connect with us on
Nature network - http://network.nature.com/groups/euroscicon/
- http://www.linkedin.com/groups?gid=1939569
- http://www.facebook.com/group.php?gid=70847076549
- http://twitter.com/Euroscicon/
About the Chairs
Claudia Mauri graduated magna cum laude in 1984 from University La Sapienza in Rome. She worked as a Post-Doctoral Fellow at The Kennedy Institute of Rheumatology. She moved to University College London in 2002 where she established her group. She holds a readership position in immunology/rheumatology. Her research interest lies in understanding the mechanisms driving autoimmunity with a particular interest in understanding the function of regulatory B cells in experimental models of rheumatic disease and in patients with Systemic Lupus Erythematosus and Rheumatoid Arthritis.
Robert Barker holds a personal Chair in Immunology and leads the Immunology and Inflammation Research Programme at the University of Aberdeen. His research has for many years focused on the study of immune-mediated diseases, using red blood cells as model target antigens. The lessons learnt have now been extended to further understand the pathogenesis of a wide range of diseases in which the immune system plays an important role, including autoimmune haemolytic anaemia; haemolytic disease of the newborn; immune-mediated thrombocytopenia; Goodpasture’s disease; bullous skin diseases; atopy and asthma; viral and tumour immune evasion. The aim is to be able to control these diseases by manipulating immune regulation, particularly as mediated by regulatory T lymphocytes, and a number of projects are now undergoing commercial development for human trials. Professor Barker is currently a Trustee of the British Society for Immunology, the Groups’ Secretary of the British Society for Immunology, and a British Society for Immunology Autoimmunity Affinity Group Committee Member. He also serves as a member of the Research Committee of the Arthritis and Rheumatism Campaign.
Sponsors
About the Speakers
Michael Ehrenstein is Professor of experimental rheumatology at University College London (UCL), UK. Between 1995 and 1999 he worked at the Laboratory of Molecular Biology in Cambridge, UK. He leads a research group investigating the roles of B and T cells and their products in promoting and regulating inflammation and autoimmunity, and how novel therapies modulate the autoimmune response in the context of rheumatoid arthritis and systemic lupus erythematosus.
Leonie Taams,is a Senior Lecturer in Immunology at King’s College London. She obtained a PhD in Immunology from Utrecht University in the Netherlands, after which she worked as a postdoctoral fellow with prof Arne Akbar at UCL and with prof Floris Lafeber and prof Hans Bijlsma at the University Medical Centre Utrecht, NL. The Taams lab is interested in investigating the regulation of inflammation in humans. The lab has a specific interest in the cross-talk between CD4+ T cells subsets and monocytes, and in the role of Th17 cells in the pathogenesis of rheumatoid arthirits.
Elizabeth Jury, an Arthritis Research UK Career Development Fellow, has worked at the Centre for Rheumatology Research, UCL since 2000. In this time she has opened up new avenues of research into signalling abnormalities in T and B cells from patients with SLE and RA making significant contributions towards understanding the nature of these abnormalities and how they relate to disease pathogenesis. The main focus of her research is to understand the role of plasma membrane, cellular and serum lipids on immune cell activation with the long-term aim to identify new targets for development of novel therapeutics.
Marc Veldhoen trained in Medical Biology at the Faculty of Medicine, Utrecht University, and continued his scientific career at the Division of Molecular Immunology at the National Institute for Medical Research in Mill Hill, London. He was the first to describe the de novo differentiation of the new Th17 as well as the Th9 subsets of T helper cells. He went on to show the importance of Th17 cells in the initiation of autoimmune responses and, via the identification of the Aryl Hydrocarbon Receptor in Th17, established a link between environmental toxins and auto-immunity.
Lucy Walker is a Reader in Immune Regulation and Autoimmunity at the Unviersity of Birmingham. She has a longstanding interest in T cell costimulatory pathways and the regulation of autoimmune diabetes. During a 3-year fellowship in Professor Abul Abbas’s lab at Universitcy of California San Francisco (UCSF) she generated a transgenic model to study antigen-specific regulatory T cells. On her return to the UK in 2004 she was awarded an MRC Career Development Award, and subsequently an MRC Senior Fellowship, to study T cell differentiation and regulation in autoimmune diabetes.
Dont forget to sign up to Euroscicons’ e-newsletter at www.euroscicon.com/signup.htm to keep up to date with European Life Science news and events and to be notified of the follow up to this event
Registration Web Site: www.regonline.co.uk/autoimmune11
Post expires at 8:39am on Friday March 11th, 2011